HIPAA-compliant Software Development for mHealth

Smartphones and wearables are widely used for telehealth, and even hospitals and insurance companies’ adoption of mobile devices is growing. Simultaneously, data breaches in the healthcare sector pose increasingly serious problems. The developers of mobile healthcare apps or software for wearable devices (mHealth) need to understand the relevant laws that regulate patient privacy and the health data security.
In the U.S., these issues fall under the purview of HIPAA (meaning Health Insurance Portability and Accountability Act of 1996). It governs the management, storage, and transmission of protected health information (PHI). Since September 2013, all doctors, hospitals, insurers, and other entities that deal with storage, management, recording, and passing PHI, e.g., build mHealth apps, have been obliged to follow HIPAA guidelines to ensure compliance.
Healthcare app developers are primarily interested in the HIPAA Privacy and Security Rules published by the Department of Health and Human Services (HHS). The first requires protection for certain patient health-related information that is transferred or stored in electronic format. The second outlines several safeguards whose implementation is necessary for HIPAA compliance.
The efforts of software developers and other players to meet the national standards set in the Rules are overseen by the HHS Office for Civil Rights (OCR). It’s worth mentioning, however, that there is no governmental structure responsible for formal HIPAA certification of organizations and products.
Nevertheless, the legislation gave rise to a whole industry encompassing HIPAA training for the employees, audits, consulting, legal assistance, and more. These activities are increasingly important in the light of significant losses that improper handling of patient data or neglecting HIPAA requirements entail.
This article offers advice to help a healthcare or health insurance app meet those requirements so that it becomes popular, profitable, and doesn’t subject you to the OCR sanctions. Many of the tips will be relevant for apps targeting other countries as well.
The first step is to understand all applicable terms and whether HIPAA software requirements apply to your mHealth app in the first place.
Applications that Require HIPAA Software Compliance
To gauge a mobile or web application against the need for HIPAA compliance, two criteria are considered:
- the type of information it generates, shares, or stores
- the type of entity the software deals with or is intended for
Information
The healthcare software domain interacts with two types of information:
I. Consumer health information (CHI).
This type includes data that apps can gather from a fitness tracker, e.g., heart rate readings, the number of steps walked, calories burnt, etc.
II. Protected health information (PHI).
This class encompasses virtually any data that can be used to identify a patient. PHI consists of health data and personal identifiers. The first relates to a patient’s physical or mental health or condition and the payment details for the provision of healthcare. This may include doctor bills, emails, lab test results, MRI scans, and other data that is created, utilized, or disclosed in the course of providing healthcare services. Information related to healthcare insurance coverage for medical patients and even geolocation details that locate a person within a territory smaller than a state also constitute health data.
The mere fact that an individual has received medical services may count, but health data becomes PHI only in combination with personally identifiable information.
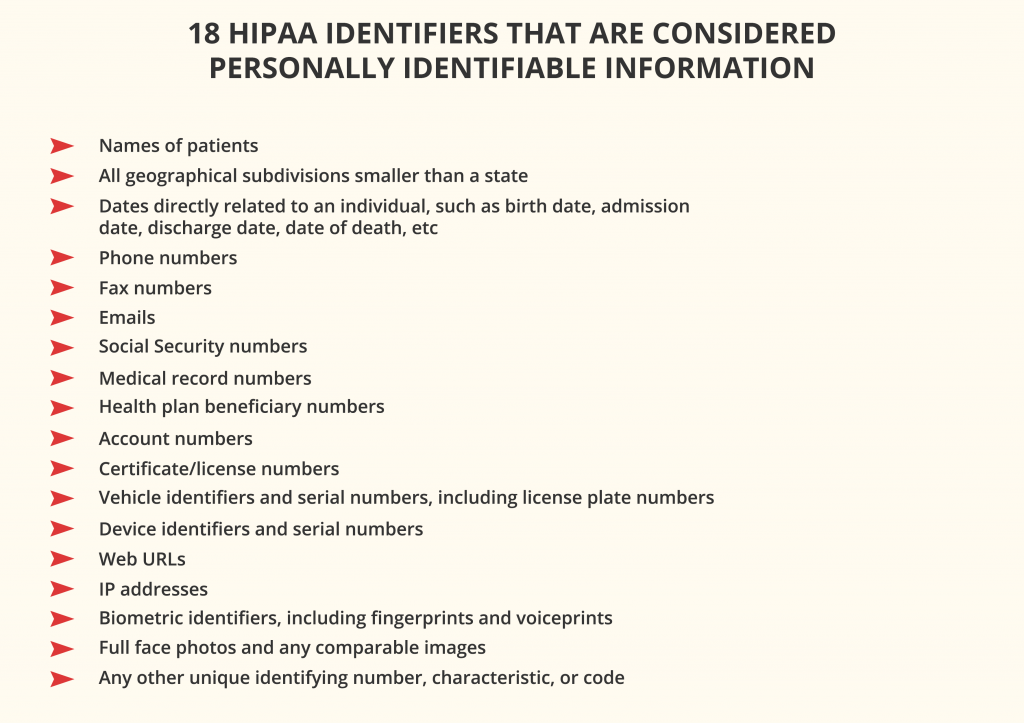
The rule of thumb is: if an application collects, processes, stores, or transfers any PHI, HIPAA software compliance is mandatory. Even if it contains a user’s profile with their first and last name that can be traced back to a particular patient, the app must comply. The same applies when sensitive data is stored on a third-party server.
Entities
According to Privacy Rule, two types of organizations are subjected to HIPAA law compliance:
I. Covered entities
Covered entities include:
- all healthcare providers that conduct financial and administrative transactions for which HHS has adopted a standard. These may be hospitals, clinics, nursing homes, pharmacies, private practices, dentists, psychotherapists, chiropractors, et al.
- health plans, such as health insurance companies, health maintenance organizations, company health plans, government programs like Medicare and Medicaid, and the military and veterans health care programs
- clearinghouses that act as middlemen between the healthcare providers and insurance companies and process non-standard health information received from those entities
The covered financial transactions include fund transfers, electronic billing, etc.
If your app is intended for use by a covered entity, more than likely, you will have to comply with HIPAA. If it facilitates doctor-patient interactions, it needs to comply because doctors and the hospitals they work for are covered entities. HIPAA software requirements may be applicable even to apps that deal with employee records for hospitals and education records for medical institutions.
II. Business associates
These persons or organizations collect, store, process, or transmit individually identifiable health information as part of a service to, or on behalf of, a covered entity. This category may include lawyers, accountants, billing firms, software providers, developers of healthcare apps, hosting/data storage providers, email services and email encryption providers, and other third parties that may process patients’ data.
It may seem that HIPAA rules apply to virtually all types of covered entities and business associates who produce, access, process, or store PHI, even if they do so unintentionally. The following instruments may prove useful when app developers are in doubt as to the laws and regulations to follow:
Anybody who qualifies as a covered entity or business associate must:
- Implement the appropriate administrative, physical, and technical safeguards laid out in the HIPAA Security Rule to ensure the confidentiality, integrity, and security of electronically transmitted PHI (ePHI).
- Minimize the use and sharing of PHI to the extent required to accomplish the intended task.
- Minimize the number of entities and individuals who can access patient information and implement HIPAA training programs for the staff on protecting such information.
- Sign a business associate agreement (BAA) with each party that has access to its PHI to ensure the security of PHI and overall HIPAA compliance.
Now, let’s focus on HIPAA software requirements that are critical for web and mobile app developers.
Requirements for HIPAA-compliant Software Development
Software developers and IT service providers that deal with HIPAA-covered entities and PHI should strive to implement all applicable administrative, physical, and technical safeguards mentioned above.
For example, the physical data standards cover physical access to ePHI, whether it’s stored in the cloud, in a remote data center, or on-premises servers and even equipment: PCs, laptops, tablets, or smartphones. They require protection of the back-end, a network for data transfer, and ensuring that ePHI cannot be compromised if mobile devices are hacked, lost, or stolen.
Nowadays, much of the burden of physical security standards has been taken over by HIPAA-compliant cloud hosting companies like Amazon Web Services (AWS), Firehost, Rackspace, or TrueVault. Other aspects are handled by software developers’ internal rules around who can and can’t access PHI and manage access to the data. You can find basic information relating to the administrative safeguards and physical data security here.
This article is primarily focused on HIPAA information technology requirements that distinguish the development of HIPAA-compliant mobile apps from other types of software. The modifications in the development process, app features, and design are mostly related to the technical safeguards – the ideal workflow an app must follow in handling ePHI.
The applicable requirements and best practices can be divided into three groups:
1. Access control requirements:
- Assigning unique user identification code/number/name for tracking user identities
- Established procedures for getting access to required ePHI in case of an emergency, e.g., power failure
- Verification of the identity of a person that requests access to ePHI via a password or PIN, smart card, key, or biometric data
- Automatic logging users off of computers and devices after a certain period of inactivity
- Encryption and decryption of ePHI data at all stages
2. Transmission security:
- Security measures for eliminating the chances of undetected data modification by unauthorized persons
- Encrypting ePHI during transmission wherever required
3. Audit and integrity standards:
- Hardware, software, and procedural mechanisms for tracking, recording, and examining activities in systems using or storing ePHI
- Policies, procedures, and solutions that prevent ePHI from unauthorized modification or destruction
The technical safeguards directly determine the technology employed for protecting and controlling access to ePHI that can be transferred between or stored on servers and devices. For example, the technical policies for HIPAA compliance require that ePHI at rest and in transit should be encrypted when it passes beyond an organization’s internal firewalled servers. This ensures that even if a data breach occurs, intruders will be unable to read, decode, and use this data. However, the law doesn’t explicitly specify any technologies to use.
Before we delve into the specifics of HIPAA-compliant app development, it will be useful to recollect why businesses put up with the increasing complexity and cost of HIPAA compliance.
The Growing Need for HIPAA Compliance
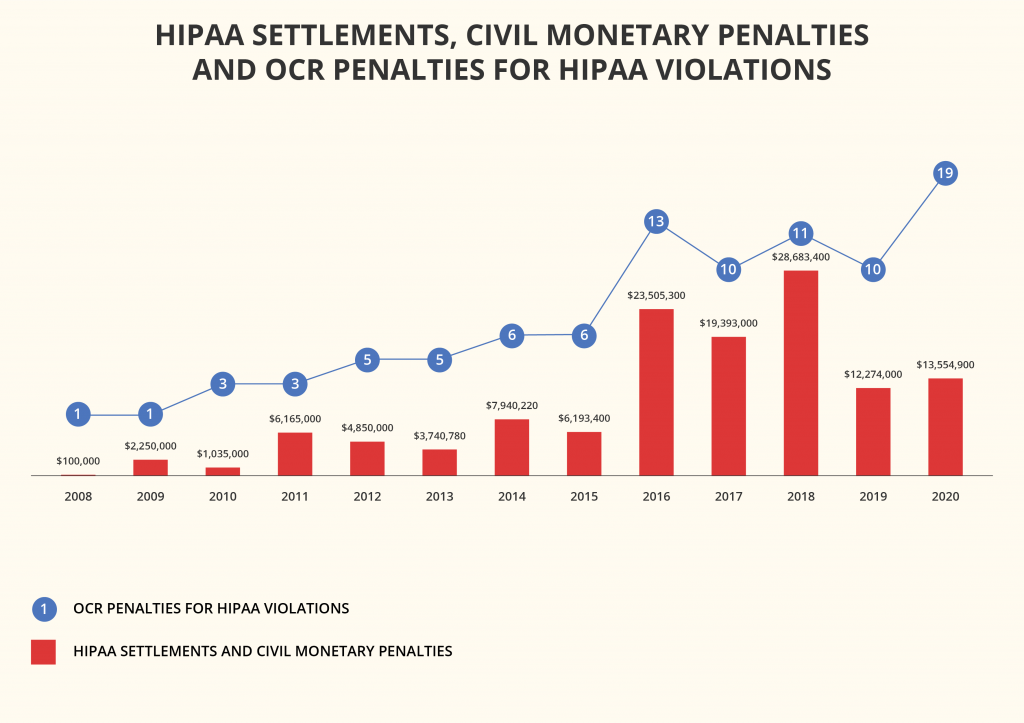
What is HIPAA compliance all about? The benefits for healthcare providers and patients, such as identity theft prevention, are undeniable. The HIPAA requirements also urge software developers to build future-proof infrastructures and come up with innovative solutions for the mHealth market. However, the biggest concern of businesses and institutions is to minimize the financial risks.
HIPAA compliance mistakes come at a high price. For example, cloud security company Bitglass analyzed data from HHS’ database and released a report that revealed that in 2020, healthcare data breaches grew 55.1% from 2019 and affected more than 26 million people. The average cost per breached record has risen too.
The leading causes of security breaches were:
- hacking and IT incidents, which accounted for 67% of all healthcare breaches in 2020;
- unauthorized disclosure, which led to 21.5% of breaches;
- loss or theft of devices, accountable for nearly 9% of breaches.
The penalties for healthcare providers bypassing the HIPAA compliance rules and regulations start from $100 per violation. If a data breach occurs due to non-compliance with HIPAA, each person whose data was exposed makes a separate case, although the fines aren’t to exceed $1.5 million per year for one category.
Healthcare organizations are already facing enormous fines for insufficient security of their devices or software. A prominent example is the $3.2 million fine imposed on Children’s Medical Center of Dallas for failing to encrypt and protect portable devices.
In 2020, the average cost of breaking HIPAA compliance rules and regulations for healthcare organizations was $713,415.
For startups, such consequences of non-compliance in healthcare data protection can prove deadly. Luckily, even new app developers can leverage the wealth of knowledge amassed by experts and follow the best practices and recommendations formulated over the years.
Best Practices for Organizations to Promote HIPAA Compliance
Healthcare providers, insurers, health tech companies, and other entities are recommended to complete several steps to become HIPAA-compliant.
1. Adopt the minimum necessary rule
This best practice can be formulated as follows:
- Do not collect more data than you will need
- Don’t store data for longer than is required for your work
Continually assess how much information your app actually needs to operate and bring value to the users. An entity that gathers and keeps superfluous information not only fails HIPAA standards but also wastes resources on this data storage and protection.
According to the HIPAA Privacy Rule, no person should see more information than their job requires. (The rule also specifies the patient’s rights to view and grant or restrict access to their own information.)
HIPAA compliance is easier to achieve when all trackable data collected from users is cloud-based and stored in secure servers. Eliminate unnecessary collection and storage of user data. Track only the data that you really need and exclude from your analytics any data that may violate HIPAA rules. Reasonably limit the sharing of PHI to the minimum required to accomplish the intended tasks.
2. Separate the PHI
Figure out which of the data can be categorized as PHI and see what PHI you can avoid storing or transferring through your mobile app.
It’s recommended that all patients’ health data should be kept in a separate database, away from other app data. That way, you can avoid constantly encrypting and decrypting every byte.
3. Involve the personnel
Teach your staff to recognize cyber-attacks, take the necessary precautions, and report security incidents. You also should have a sanctions policy in place for employees violating HIPAA regulations.
The above-mentioned administrative safeguards dictate the appointment of a security officer and a privacy officer that will be responsible for establishing measures for data protection and management of employee behavior. The security officer must regularly perform risk assessments, defining the organization’s vulnerabilities, risks, and threats to the availability, confidentiality, and integrity of all PHI that it produces, obtains, maintains, or shares.
4. Perform an initial risk analysis
Namely, a company should:
- determine where PHI comes from and where it is stored, maintained, and transferred
- identify and document possible risks entailed by your existing vulnerabilities
- define vulnerability risk levels and the possible impact of each one
- evaluate the security practices that are in place to protect PHI
- check whether the present security practices are used correctly
- assess the potential impact of a PHI breach that might occur
- define the most suitable audit controls for your systems that contain or use ePHI
- prepare and share across the organization a report of the risk analysis
- develop an actionable plan including measures to improve PHI security
Once you have the results, you can proceed to adjust the organization’s processes to address the issues.
5. Eliminate HIPAA compliance risks and adjust processes
Start with solving smaller non-conformities and gradually proceed to larger ones. For example, the first steps may include implementing two-factor authentication, signing a BAA with your backup provider, or training the staff on cybersecurity measures, permitted uses, and disclosures of PHI. Then, you can start working towards more complex goals, always coupled with relevant HIPAA training for the employees.
6. Dispose of PHI properly
PHI that is no longer needed should be disposed of permanently, i.e., erased. As long as a copy of such PHI remains in one of your backups, the data isn’t considered “disposed of.” Archived and backup data can also hide in photocopiers, scanners, biomedical equipment like MRI or ultrasound machines, laptops and other portable devices, memory cards, USB flash drives, DVDs/CDs, flash memory in motherboards and network cards, ROM or RAM, and even floppy disks.
Developers should take measures to dispose of all the unused data in a safe, non-retrievable manner. They should also properly destroy the media that contain PHI before throwing or giving them away. In flash-based memory drives, such as USB sticks, data is spread over the media, making it difficult to erase sensitive information with regular data destruction software. In this case, manufacturer utilities like Samsung Magician can help you dispose of your flash drives.
7. Make HIPAA compliance a long-term strategy
Becoming HIPAA-compliant is an ongoing process, especially in the light of the growing interoperability in healthcare. Your software product or products will keep evolving, and so should their security.
Focus on the HIPAA requirements from the initial stages of your mHealth app development and check if you need to comply with any other privacy and security regulations before you start.
Document all your efforts to protect PHI throughout the development process and beyond.
Regular technical and non-technical evaluations of such efforts will be required. The regulator has published an audit protocol that can help you assess your HIPAA compliance.
Set up procedures for monitoring HIPAA issues as you go. You will need to track PHI access, detect security issues, regularly reevaluate the effectiveness of security measures, and assess potential risks to compromising ePHI.
For each release of your app, provide specifications, plans to test its security, and their results.
For continuous management of potential security risks, it may be beneficial to employ network monitoring software. As a minimum, such tools can track logins into the system and, at maximum, provide automated compliance reporting.
The following chapter will describe some app features supporting compliance with HIPAA and technology that software developers can leverage to implement such features.
mHealth Features and Solutions that Promote HIPAA Software Compliance
The minimum list of features that are essential to HIPAA-compliant products includes the following:
1. Data access control
Any system that stores PHI should restrict viewing and alterations to the information.
Role-based access control allows app developers to implement those restrictions by granting to groups of users, e.g., doctors, lab technicians, administrators, et al., privileges essential to their jobs.
Another way to accomplish this is to assign a unique ID for identifying and tracking the activities of each user accessing your system. Then, you can grant each user a set of privileges allowing them to view or modify specific data, and then regulate access to individual database entities and URLs.
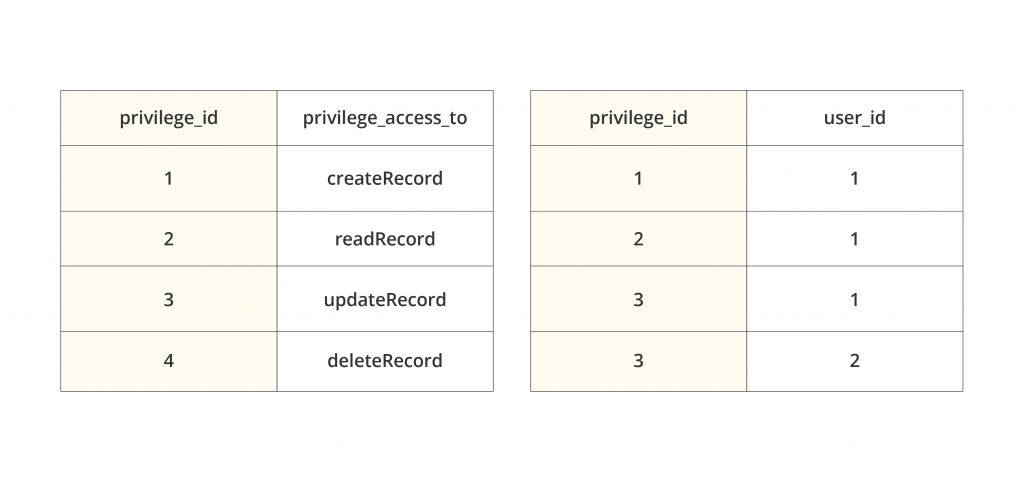
The simplest form of user-based access control consists of two database tables: the list of privileges with their IDs and the distribution of those privileges to individual users. In the above case, a doctor (user ID 1) is entitled to create, view, and update medical records; the lab technician (user ID 2) can only update them.
After assigning privileges, app developers need to enforce regular authentication and preclude access to the system without authentication.
2. Person and entity authentication
Several ways to implement proof of identity in a HIPAA-compliant way are recommended:
- Password or Personal Identification Number (PIN). Unfortunately, the bulk ofdata breaches happen due to weak or stolen passwords. To reduce such risks, healthcare apps should:
- require secure passwords that consist of at least eight characters, including capital letters, numbers, and special symbols, and excluding the commonly used vocabulary words and combinations, such as “password,” “qwerty,” or “123456”
- preclude the use of the username variations
- prevent password reuse
Your app may check these requirements on the signup screen and decline weak passwords.
- Biometrics (e.g., fingerprint, face ID, or voice patterns). For a better authentication process and user experience, it’s helpful to offer fingerprint authentication: it will also protect sensitive data if a device is lost or stolen.
- Physical means of identification, e.g., smart card, key, or token.
Multi-factor authentication combining a secure password/PIN with other verification methods reinforces an app’s security. The second element can be anything from a one-use security code received via SMS to a biometric scanner. The idea is simple but effective: if hackers obtain a user’s password, they’ll also have to steal their device or fingerprints to access sensitive data.
However, even secure authentication isn’t enough. Hackers can get between the user’s device and your servers and access the PHI without compromising the account. A digital signature may be helpful against such session hijacking. Re-entering the password when signing off on a document would prove the user identity.
Other ways to ensure that only authorized personnel can access the data include regular change of passwords by employees and access control audits.
3. Access during emergencies
An emergency occurs when a natural or man-made disaster renders electrical power systems, hospital management, and other systems inoperative, disrupting the essential services and networks. However, healthcare providers should be able to access ePHI under all circumstances.
Neither should authorization get in the way of aiding patients in an emergency. For example, a doctor may need to urgently view a patient’s records. It’s reasonable to allow authorized users to access any data they need when the situation requires so while the system automatically notifies several other people and launches a review procedure.
4. Automatic logoff
A system containing or using PHI should automatically terminate a session after a specified period of inactivity in the app, around 2-3 minutes. This protects PHI in the case a user loses their device while logged in. To continue, a user would have to re-enter their password or be verified in another way.
5. Encryption/decryption
The encryption of all communications with the apps and data is the best way to ensure PHI integrity. Whether the data is at rest locally on smartphones, stored with a SaaS or cloud server, or travels between apps and servers, it needs encryption. Even if hackers steal patient data, it will make no sense to them without the decryption keys.
If your app asks for sensitive user data, you need to embed a system for automatic encryption of all the data, whether it is stored locally or transmitted to a central server.

For the encryption of data stored in the software system – backups, databases, and logs – experts can leverage RSA and AES algorithms and encrypted databases like SQLCipher.
For the end-to-end encryption of data during transmission, you can use services like AWS’ Amazon S3 or Google Cloud that run Transport Layer Security 1.2. TLS can be enough by itself, but AES 256-bit encryption can fortify it further.
Gmail doesn’t provide the necessary protection for PHI sent via emails. If you send emails beyond your firewalled server, they need to be encrypted. You can use browser extensions, the OpenPGP encryption method, or a HIPAA-compliant email service like Paubox that can do the job.
iOS and Android devices tend to store that data on disks when the network is offline. This reinforces the requirement for the proper encryption of data that is at rest on devices.
All parties should also encrypt the hard drives of all devices that contain PHI. Encryption tools like BitLocker for Windows or FileVault for Mac OS can do this.
6. Secure PHI transmission
To protect the PHI that circulates over the network and between the different tiers of the system, app developers also need secure connections and protocols.
To this end, they should force HTTPS at least for the signup screens, all pages containing PHI and authorization cookies, and ideally for all communications. This secure communication protocol encrypts data with TLS.
App developers need to get an SSL certificate from a trusted provider, properly install it, and make sure to use a secure SSH or FTPS protocol to send the files containing PHI instead of the regular FTP.
During client-server data transfers, when the data has to be transmitted in the body of the POST requests, the system may first encrypt them on the sender’s side and decrypt on the receiver’s side. This helps prevent man-in-the-middle attacks.
For data in transmission, using SSL-enabled endpoints with Amazon S3 is the best option. Some features include EC2 AMI Creation or Snapshotting.
When the information is in transit between a device and server, you can use modern cipher suites and TLS to handle data on the move. When the devices operate in untrusted networks such as public Wi-Fi, the app can use the certificate pinning process.
The developers also need to embed a Virtual Private Network (VPN) for greater file security during data transfers. Another level of certification is Health Level 7 (HL7) that provides data transfer guidelines among healthcare providers.
Make sure your app doesn’t send any push notifications containing PHI. They aren’t secure by default, appearing on the screen even when it’s locked. The same applies to other automatic messages.
Apps should also avoid
- the transmission of PHI via SMS and MMS because they are not encrypted
- transmitting PHI via emails (or at least limit the information that can be shared this way)
- leaking the data into backups and log files that are vulnerable when using SD cards on Android devices.
Once the data has landed in the server storage, the provisions around the key rotation, key management, encrypted backup, and audit logging come into play.
7. Data backup and storage
Backups are essential for data integrity. Multiple copies have to be safely stored in several different locations, but only of those pieces of data that you absolutely have to keep. Avoid storing or cacheing PHI whenever possible, e.g., users’ geolocation data (other than state-level).
All information with a high or medium risk of data compromise should be backed up daily and stored in a secure facility.
The backups themselves and the cloud services that healthcare apps are connected to should also comply with HIPAA security standards. Major cloud providers, such as AWS, Aptible, Datica, Google Compute Engine, and TrueVault, help a lot by offering out-of-the-box HIPAA-compliant back-end, backup, and recovery services.
Continuously log your system’s downtime and any failures to back up the PHI; test the system regularly to prevent recovery failures.
The app should automatically sync data between a local device and central servers so that a user doesn’t always have to stay connected to a network for accessing data.

There also should be an option for patients to erase their data from the system, including remote removal from a lost mobile device.
8. Audit controls and activity logs
For the organizations to know who, when, and where accessed, updated, modified, or deleted PHI from their system, the system must record each time a user logs in and out, their IP Address, point of entry, and what exactly data was accessed. It should store and present activity logs recording the users’ interactions with the data in a human-readable format.
For recording all interactions with the information, developers may use a five-column table in a database or a log file. These columns should be:
- user_id. The unique identifier of a user who interacted with PHI
- entity_name. The entity with which the user interacted. (An entity represents some real-world concept in your database, such as a health record)
- record_id. The entity’s identifier
- action_type. The nature of interaction (create, read, update, or delete)
- action_time. The precise time of interaction
The app architecture should incorporate systems that enable security providers to access detailed logging information. Periodic audits of the activity logs should help discover if any users abuse their privileges to access PHI. It’s helpful to set up emergency alarms in the case of a system anomaly or abnormal system behavior.
AWS CloudWatch is excellent at keeping a record of access to PHI. It allows viewing the access data as graphs, running constant analytics, and stringent HIPAA security risk profiling.
Regarding the AWS levels of access, AWSCloudTrail may be recommended. It will help you record the data (AWS API Calls). AWS Config will let you handle AWS Resource inventory,
configuration history, and configuration change notifications.
9. Extra security for mobile devices
Smartphones and tablets present additional risks because they can be easily stolen or lost, compromising sensitive information that was stored or accessible on the devices.
To prevent this, you can include into your onboarding or send via emails the instructions for users to use screen lock, full-device encryption, and remote data erasure capabilities on their Android or iOS devices.
Many physicians use personal smartphones to send health information. A secure messaging platform within your app will mitigate this risk factor. Another solution is encrypted password-protected health portals where patients can read messages from their doctors without actually any PHI in them (e.g., “Dear User, you’ve got a new message from [redacted]”).
Even all the features listed above can’t guarantee your app’s absolute security. However, having them all should convince an auditor that you’ve done enough to protect patient records and other sensitive information in compliance with the HIPAA requirements.
Further Tips on Building HIPAA-compliant mHealth Apps
The entire software development process should occur with an eye on fulfilling government requirements for healthcare applications.
Hire experts
Don’t attempt to meet all HIPAA requirements on your own if you don’t have enough expertise or experience. It’s always better to hire third-party experts to consult, review your existing app architecture, analyze your current HIPAA-compliance preparedness, and audit your entire system.
A qualified HIPAA or security specialist will help you understand what kinds of data you deal with qualify as PHI. This may be the first step to a new app development, allowing to design the future database properly. The expert can also advise on what kind of data you can avoid sharing through your mHealth app and define the security requirements for it.
Outsourcing the HIPAA-compliant software development to an agency with a corresponding track record also can solve this problem while saving costs. Experienced healthcare app developers will build your product faster, and the hourly rates of remote developers are often considerably lower than in the US. This is a bonus both for startups and established health tech companies and healthcare providers.
Another good practice is to outsource testing to a third party that can audit your app developers’ work by running all necessary tests.
Upon release, you can periodically hire professionals to audit your app’s infrastructure and code.
Use third-party solutions that are already HIPAA-compliant
Instead of trying to build a HIPAA-compliant mobile app from scratch, it’s reasonable to take maximum advantage of high-quality, third-party solutions and ready-made infrastructure that are already HIPAA-compliant. This is called IaaS – Infrastructure as a service – and dramatically saves time, money, and effort.
Leading hosting providers take responsibility for security while storing or managing PHI data, and you won’t have to worry about signing a BAA with them. AWS and TrueVault are good examples of such HIPAA-compliant technology you can use for healthcare software development.
Continually monitor, maintain, and test your mHealth app’s security
Establish a long-term strategy for monitoring all HIPAA-related aspects of your mobile app.
After your mHealth MVP has been developed, test it thoroughly with fake users and data to ensure security, particularly the gateways and authorization processes. Then, you will need to perform testing and validate your app’s security after every update. Test it both statically and dynamically, consult with experts, and make sure the documentation is up to date.
Maintenance is another ongoing process. Libraries, tools, frameworks, and third-party services are constantly being updated. Make sure you are using the latest version to prevent operation issues and security breaches.
Here are some more tips on how to deal with mobile apps:
- Use an efficient privacy policy that clearly explains how you treat the patients’ health data.
- Follow secure mobile development best practices, such as OWASP Mobile Top 10.
- Blockchain technology may prove helpful for the prevention of tampering with patients’ data.
Final Words of Wisdom
In 1996, the U.S. Congress enacted HIPAA, meaning, among other things, to help protect patient information from theft and fraud.
Nowadays, the consequences of non-compliance in healthcare may be disastrous and cost a fortune. The penalties for violating HIPAA rules alone start from $100 and may reach $1.5 million per year.
To minimize this risk, a healthcare company can hire a third-party agency to audit or consult them, provide the appropriate instruction, and even issue a corresponding certificate. However, remember that being HIPAA-certified does not equal being HIPAA-compliant; it means only that a company has completed a training course on becoming compliant. Moreover, OCR doesn’t recognize any third-party HIPAA certification either.
Finally, such outsiders’ services may be useless if you engage them after building your software without proper administrative and technical policies for HIPAA compliance. The best way to promote your mHealth product’s compliance is to address those requirements from day one.
HIPAA-compliant software development requires that infrastructure should be set up to ensure safe collection, storage, and transfer of sensitive information and prevent its alteration by unauthorized parties or by mistake. Measures like access authorization combined with distinct user roles and access rights to different app features, data encryption, and regular backups are indispensable when HIPAA-compliant mHealth apps are built.
Whether it is mHealth, SaaS, eCommerce, or FinTechapplication development, Alternative-spaces will safeguard the users’ data under any conditions. Our team is experienced in building apps that meet all applicable federal and international security and privacy requirements.
Please feel free to book a free consultation if you have questions about the HIPAA compliance of your product or want software design and development services.
Content created by our partner, Onix-systems.
 Home
Home