Why and How to Achieve Interoperability in Healthcare IT

This article aims to form an understanding of health information technology interoperability, including
- the definition and examples of healthcare technology interoperability
- its benefits for patients, healthcare facilities, and healthcare providers
- major challenges to interoperability implementation
- some methods for doing it smoothly and effectively
The article also includes references to Alternative-spaces’ experience building healthcare apps. Whether you are a healthcare business or a MedTech startup, it’s worthy of your attention.
What Is Interoperability in Healthcare Information Systems?
Today’s healthcare technology is a mix of systems, databases, devices, applications, and processes. Organizations and professionals keep integrating new information technology into care delivery, learning, patient engagement, management, and other processes to improve patient care while maximizing operational efficiencies, lowering costs, and staying competitive.
Patients also expect a seamless customer experience, better security, and more innovative services. In particular, they want their health records at their fingertips and don’t want to carry their information from one healthcare provider to another.
To meet these challenges, hospitals, doctors, insurance agencies, research institutes, and IT providers need to develop new ways to communicate with patients and each other’s computerized systems. This need is reflected by the concept of interoperability in healthcare.
Generally, interoperability refers to the ability of disparate hardware, software, applications, databases, and other computer systems, often coming from different manufacturers and vendors, to connect, communicate, and share each other’s data without any restrictions, to interpret that data similarly so that it becomes information, and to use that information.
In the context of healthcare, it may mean the extent to which health information systems, devices, or apps can connect within or outside a healthcare organization and access, securely exchange, and use patient data and other information: admission and discharge records, transfer notifications, lab and examination results, filed claims, and so forth.
It may also mean the ability of patients, clinicians, hospitals, private practices, labs, pharmacies, researchers, and other actors to quickly exchange and use information across apps, wearables, etc., for effective delivery of healthcare for individuals, communities, and the entire population.
In the US, the issue of interoperability has been around since the Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted in 2009. It set the meaningful use of interoperable electronic health records (EHR) as a critical national goal.
Achieving this goal requires that hospitals and physicians should be capable of health information exchange (HIE). Compliance with interoperability rules also means not interfering with patients’ access to, or use of, their electronic health information and refraining from information blocking.
The American Healthcare Information and Management Systems Society (HIMSS) defined the following levels of health IT interoperability:
1. Foundational
This is the initial level of data sharing between separate information systems. Foundational interoperability ensures that one system can connect to and share data with another system. The receiving system needn’t interpret the data with extra technologies or user intervention.
2. Structural
This tier is also known as syntactic or technical interoperability. It defines the format and structure of the data to exchange allowing the receiving system to interpret it at the level of data fields, e.g., patient records. This has to do with the standards that govern the format of messages exchanged between systems to preserve the unaltered clinical or operational purpose and meaning of the data.
3. Semantic
Semantic interoperability ensures that two or more systems or components can share, fully interpret, and immediately use the exchanged information. It utilizes the structuring and codification of the data to support patient information exchange among authorized parties via potentially disparate EHRs and other systems. It’s vital for eliminating the existing technology and terminology gaps between the numerous software systems and data sources.
4. Organizational
This level encompasses social and organizational aspects and data exchange policies necessary for introducing interoperability to entities’ workflows and facilitating smooth and secure data exchange.

The interoperability goals of the US HHS’ Office of the National Coordinator (ONC) imply:
- Patients’ effortless access to their health information electronically;
- Access to population-level health information for providers and payers responsible for managing benefits;
- The use of open and accessible application programming interfaces (APIs) to encourage user-focused innovation to increase the accessibility of health information and EHR usability.
Examples of Interoperability in Healthcare
Organizations and individuals help improve interoperability in healthcare when:
- Patients shop for healthcare services and insurance on their smartphones.
- A web or mobile application streamlines a patient’s experience across the customer journey and enables smarter decision-making as they find, receive, and pay for care.
- Patients can view their EMR (electronic medical records) on patient portals.
- Hospitals send event notifications regarding admission, discharge, and transfer to other healthcare providers.
- A healthcare organization stores patient data from a chronic disease management app on virtual private servers so physicians can access it anytime, even on their smartphones.
- A mental health app shares a patient’s health data with their healthcare providers’ EHR/EMR.
- Hospital networks, suppliers, and emergency stockpiles regularly enter standardized data into an application for monitoring personal protective equipment inventory, which will enable decision-makers to track their routine PPE use and have accurate information during emergencies, such as pandemics.
- Documents are exchanged over federated repositories.
- Medicare Advantage, Medicaid and Children’s Health Insurance Program FFS, Medicaid and CHIP managed care, and QHPs on the FFEs can access patient healthcare claims and clinical information through standards-based APIs.
- An omnichannel platform enables payers to communicate with their members via emails, text, online portals, and mail.
- Payers exchange patient data from their systems upon request…
… and other cases where data is made usable, immediately available to share, and intelligently interpreted and presented to recipients, information systems are connected and integrated, and all forms of healthcare are enabled to tap into the existing wealth of information.
A Few Benefits of Healthcare Technology Interoperability
The lack of HIT interoperability entails inconvenience for the patients at best. Patient records still rely heavily on the forms they fill out. This results in inaccuracies and inconsistencies contaminating EHRs, healthcare providers unable to access patients’ complete information, and a high percentage of patients not matched properly to their records when seeking care. Manual data input errors may even put a patient’s health and safety at risk.
As opposed to that, patients and healthcare providers are likely to reap multiple benefits from interoperability:
Greater convenience and control for patients
Interoperability implies that providers directly put personal health information conveniently in the patients’ hands, e.g., via patient portals. Having proper access to and control over that data via chosen mobile apps and regardless of a health system or type of EHR, patients will be able to make more informed decisions. Quick and easy access to their own treatment plans, lab results, and other medical records will enable them to better care for themselves.
Improved healthcare quality and patient outcomes
Connected systems can populate a fuller patient record. Having to spend less time searching for patients’ information, every healthcare professional can spend more time on patient care. When all necessary information is readily available and presented in a consistent, well-organized manner, clinicians can evaluate it faster. This speeds up decision-making, reduces errors, and facilitates treatment tailored to each patient’s genetics, preferences, and health history.
Access to complete patient records will promote the continuity of care, particularly for complex cases. Practitioners can follow up with patients quickly, providing referrals or reinforcing items related to their treatment plan. Interoperability also enables safer transitions of care, resulting in better patient outcomes.
Greater operational efficiency
By integrating software that meets interoperability criteria, healthcare providers can streamline some processes, e.g., patient identification and matching their records, reducing manual data entry, minimizing errors, and freeing up time for other tasks. By better equipping clinical staff and practitioners, interoperability enhances their productivity and reduces staff burnout.
Cost reduction
More efficient information sharing saves time and effort. Being able to share more useful information when it is needed, healthcare providers and patients can reduce the costs associated with paper-based or archaic systems, superfluous lab tests, and more.
Security and compliance
With connections to HIEs and EHRs, interoperability capabilities can ensure compliance with pay-for-performance initiatives (MACRA/MIPS), the Cures Act, and other regulations. As long as sensitive data is initially entered correctly via an interoperable network, an entity stands a greater chance of securely storing protected health information (PHI) throughout its life cycle.
Improved public health
Interoperability facilitates a quicker and more precise collection of public health data. In the ideal scenario, every healthcare provider and office would be interoperable, creating a single national or even international network. All data pertaining to patient healthcare would be shareable with any eligible hospital, diagnostic center, laboratory, etc.
For example, integrations between vendors of healthcare CRM systems and remote patient monitoring (RPM) apps can facilitate the exchange of biometric data, patient demographics, and care plan information. The analysis of collected data would empower public health agencies to predict long-term national health trends.
This paves the way for developing patient cohorts and utilizing artificial intelligence (AI) and machine learning (ML) algorithms to discover the most at-risk patient populations that require extra care. It will also be easier to recognize, interpret, track, and predict the spread of contagious diseases, prevent and control outbreaks, and increase the efficacy of treatments.
Knowing these advantages, one may wonder what stops healthcare providers, payers, vendors, and others from embracing interoperability right now. Unfortunately, they say that interoperability is only 20% technical and 80% an economic and political issue.
The Challenges to Implementing Interoperability in Healthcare IT
The primary factors that inhibit interoperability are:
Information blocking
The reluctance of insurers to cooperate with healthcare providers and disclose information is one of the main obstacles. Proprietary communication and language protocols preclude communication between different EHRs. Some vendors charge fees for transmitting data outside the system.
Lack of consistent patient identification
There is still no consistent way to identify a patient within an EHR system, let alone across a network of providers. In the US, patients are normally identified by their name, date of birth, and Social Security number. However, since different systems store each instance of this information differently, patient identification errors are possible.
A national unique patient identifier that would help recognize a patient at every point of care throughout their lifetime might solve the problem, but patient privacy concerns prevail. Thus, data privacy and security represent another barrier.

Variability of standards for exchanging and managing information
Besides different EHR formats, there are many electronic health data standards out there. They may pertain to data security, transmission, format, structure, or the meanings of codes or terms. Each standard is meant to match particular organizational needs, so clinical systems and payers use different data-sharing standards, and systems have to manipulate and sanitize data before importing it into another system.
Steps are being taken for the adoption and use of common standards for capturing, transmitting, receiving, storing, and managing patient data. Namely, to enable nationwide sharing of health-related data in the US, all key players will have to implement the following:
Fast Healthcare Interoperability Resources (FHIR)
Created by HL7 International, FHIR (pronounced “fire”) is a standardized API setting up a collection of resources that can satisfy common data exchange use cases.
FHIR can be used with apps, cloud-based systems, EHR-based data sharing, and server-based communication for structural and even semantic interoperability. It supports four data transfer paradigms, uses HTTP-based RESTful APIs suitable for mobile applications, and allows sharing documents represented in XML, JSON, and RDF format.
ONC proposed to adopt its 4th version as a foundational standard. Medicare Advantage, Medicaid, CHIP, and the federally facilitated exchanges must support this API, for example, to enable patients to access their clinical information and claims using any third-party app.
US Core Data for Interoperability (USCDI)
USCDI is a set of standardized health data classes and constituent elements for nationwide HIE. It basically outlines what pieces of information should be shared at a patient’s request.
ONC released the third version of USCDI in July 2022.
Difficulties with measuring, analyzing, and improvement of interoperability
Entities and individuals may also be confused by the lack of clear interoperability standards in healthcare: without a standardized way to measure the effects of implementation, they can’t improve it. Only the ability to measure issues across the entire healthcare chain will enable them to analyze any problem areas, make changes, and monitor how those changes improve patient care and outcomes.
Insufficient resources
The continuously changing federal and state regulations can be overwhelming for small and single practices that may not be using interoperable technology components due to the lack of resources. Not every enterprise can afford the required level of integration and communication between diverse EHR and HIT systems. For example, CMS estimated year-one implementation costs of about $4 million and ongoing annual costs around $800K for each hospital.
Human factors
Misaligned incentives and other human-centered factors can also jeopardize interoperability projects. The staff may initially meet new technology with apprehension. Clinical staff having to learn another technology can feel frustrated. The learning, double documentation, and operating between cloud-based and local platforms can seem daunting.
This list of healthcare interoperability challenges is not exhaustive, but the good news is that several solutions are feasible:
- cloud-based EHR that facilitates HIE between healthcare organizations and physicians;
- a national patient identifier that can be implemented using blockchain technology;
- use of APIs.
Cloud services offer a relatively fast and cost-effective way to create an interoperable infrastructure on top of the existing system. Some of the leading providers helping achieve interoperability in healthcare IT are Azure API for FHIR, IBM FHIR Server, Google Cloud Healthcare API, Oracle Healthcare Data Repository, and Connected Consumer Health Suite. Salesforce also built its Health Cloud and MuleSoft platform with an eye to interoperability, unlocking EHR clinical data across applications, and furthering collaboration.
Since ONC’s interoperability goals explicitly listed the use of APIs for promoting patient data access, let us dedicate a chapter to this topic.
The Role of APIs in Health IT Interoperability Implementation
Interoperability is easier to achieve if an entity’s solutions have public or open APIs. These sets of procedures and functions facilitate the development of applications that access data or features of another app or operating service. Put simply, using an API in healthcare is about enabling information systems to communicate and exchange healthcare data.
Healthcare app developers can take advantage of open APIs for the development of solutions that seamlessly connect and access the data of major EHR vendors. These APIs generally work as follows:
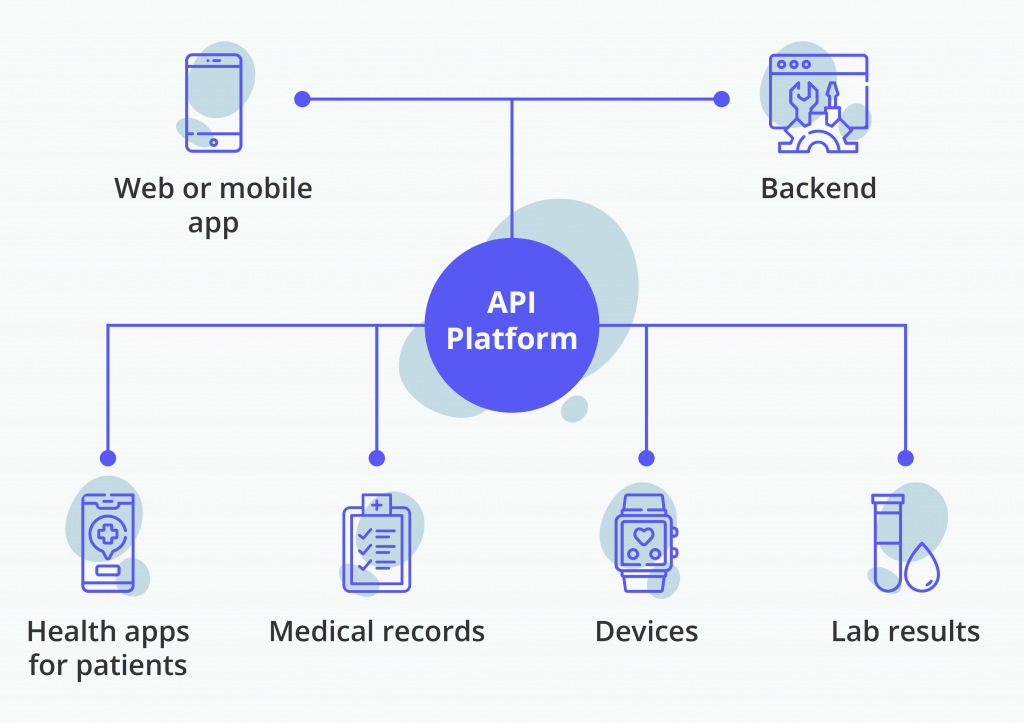
The common consumption patterns of APIs include, but are not limited to:
- Registration. These APIs are designed to manage registration-related functionalities involved with EHR systems. They facilitate a straightforward development of medical interfaces for patient portals that can be integrated with various EHR systems.
- Appointment scheduling. Such APIs allow integrating appointment booking, search for available slots, ability to cancel or rebook appointments, synchronization with other calendars, reminders, and more.
- Financial. Billing, claims, and other financial APIs help manage transactions between healthcare providers, insurers, pharmacies, and other agents. They enable doctors to create and send prescriptions to insurers or patients automatically. A financial API is essential for mobile apps where patients can pay with their smartphone.
- Hospital management. APIs of this type can handle clinical data exchange through EHR systems with different standards. An API platform that can change data formats may tap into many systems and data streams, such as patients’ treatment plans, medications, vaccinations, family health history, etc. Access to this data will empower clinicians to make better treatment decisions.
- Ancillary APIs. These APIs can consolidate information stored by a laboratory, pharmacy, telemedicine, or other auxiliary platforms, and help doctors access it.
- IoT and activity trackers. These APIs handle data streams from wearable health and activity monitoring devices in patient-centric health apps.
- Public health. These APIs promote the exchange of reportable clinical data between public or federal health registries and research organizations. They facilitate an easier exchange and access to the aggregated clinical and claims data for public health surveillance and scientists, empowering them to create hypotheses, discover trends, etc.
An entity may use a ready-made open API or develop a custom API as required by its unique needs. For instance, Healthcare Change’s data access and interoperability solutions include Clinical Document Collector API, Patient Access Clinical API and Financial API, and Provider Directory APIs.
More Tips for Achieving Healthcare Information Systems Interoperability
Providers and facilities are generally recommended to take the following steps to meet the requirements for interoperability in healthcare:
1. Review existing solutions.
Identify the level of interoperability you want to achieve for your entity and try to find out where it is now and the distance it needs to cross. Instead of entirely replacing existing infrastructure, it’s reasonable to try to expand the interoperability and squeeze maximum benefits out of it. Conduct a thorough technical review of the existing hardware, software, applications, databases, and other computer systems, as well as the processes, to understand how your data points touch the patient experience and flow into each other.
2. Engage experts.
At the first step, you will likely find out that expert help is required. Luckily, there are digital agencies experienced in interoperability software development and organizations that specialize in or count healthcare interoperability services among their primary activities.
For example:
- IBM Watson Health offers capabilities and services to help organizations as they work to follow interoperability regulations, such as
– consulting services, including interoperability maturity assessment, strategy, and development;
– IBM API Connect that supports RESTful FHIR APIs, app registration, authorization, authentication, API throttling, endpoint security, and bulk data import/export;
– interoperability solution implementation, monitoring, maintenance, requirement updates, guidance, support, education, etc.
- The Nashville-based Center for Medical Interoperability services include testing and verification of medical devices to determine compliance with selected interoperability requirements.
The earlier experts join your team on your interoperability journey, the faster and with better outcomes it will complete each subsequent step.
3. Determine your interoperability goals and strategy.
Your goals should not be limited to formal compliance with the ONC and CMS interoperability rules. It’s wise to think of interoperability as a patient-centered philosophy and long-term strategy in pursuit of leadership in your market.
Identify SMART goals of your interoperability implementation and plan the necessary resources and time-frame accordingly. Focusing on the benefits of interoperability for the organization and the patients, vendors, and other external parties, identify and document the short- and long-term expectations, including the return on investment. Be as specific as possible.

Prepare a detailed ‘implementation playbook.’ Identify the steps to be taken, outline and prioritize measurable intermediate goals, and specify how the entity will comply with applicable regulations, what interoperability standard should be adopted, what technology should be used, and any partnerships with external tech vendors or others you need to form to this end.
4. Examine workflows and determine specific use cases.
Scrutinize every type of admission, discharge, or transfer event in your entity and their respective workflows and system interactions, all clinical use cases, types of data to share, and all parties involved in providing patient care.
This research will help you determine the optimal technical approach to data transmission and how your entity can strategically use the additional data coming from other entities’ systems. Also, try to guess what cases may arise during your entity’s transition to interoperability and other transformations.
Shape a compliance roadmap with policies including what will be affected by the new rules, how to conform to state and federal law, etc.
5. Clearly communicate the objectives and methods of interoperability implementation to the stakeholders and staff.
Interoperability projects usually cut across several networks, involve many stakeholders, and require continuous motivation, top-down leadership, championship, and support at all organization levels. All stakeholders need to be on the same page about the entity’s vision of HIT interoperability, the steps to achieve it, the value expected from the initiative, the necessary resources, and the timeline.
Provide stakeholders with the implementation playbook. Explicitly communicate the current situation, the required changes, what should be achieved, and how the organization should get there. Clearly explain what interoperability means for the patients, doctors, other staff members, and the entire organization.
6. Prepare your data.
Standardized data collection and reporting that produce quality data are the keys to successful interoperability implementation. Invest in your entity’s data cleaning to make sure it’s clean, meaningful, intelligible, and will be useful to your patients. This will be beneficial to your ML and other analytics-focused efforts. If you contemplate collaborating with integration vendors, be ready to comply with their data standards.
7. Educate the staff and patients.
Education of the entity’s staff can be combined with HIPAA/HITECH and EMR training.
Healthcare providers, hospitals, and payers also need to educate patients on choosing third-party software to access and aggregate their information, about the benefits and potential risks involved in using such apps, and the dangers associated with transferring data to an app not covered by HIPAA.
After successful interoperability implementation, publicize the results.
The Takeaway
The future of interoperability in healthcare information systems revolves around data input standardization. All participants should strive to establish a standard where patient data is easily extracted, providing organizations with the most relevant and up-to-date information.
Centralizing this information across the healthcare ecosystem is another step to take. Radical interoperability, where every person’s consolidated health information will be available for research and treatment purposes, may become essential to every modern healthcare organization by 2040.
In the US, the government’s relevant initiatives aim to facilitate coordination and management, improve the quality of care, enhance patient safety and outcomes, reinforce patient privacy and security, increase staff productivity and operational efficiency, facilitate knowledge sharing and medical research, reduce medical error rates, lower healthcare costs, and ultimately, improve the entire population’s health.
The need for emerging software systems to communicate with each other will only be growing. Entities that want to satisfy patients’ demand for accessing healthcare records, shift to value-based care, or leverage analytics to maximum capacity will all need interoperability and other innovations driven by APIs.
If you plan to integrate APIs into your existing network or develop a new one within your organization’s interoperability or innovation strategy, Alternative-spaces is here to help. Our team is experienced in building medical interfaces and back-ends of different types and complexity using various cutting-edge technologies and flexible development processes.
Content created by our partner, Onix-systems.
Source: https://onix-systems.com/blog/how-to-achieve-interoperability-in-healthcare-it Home
Home